Non-Surgical Spinal Decompression Centre
Melbourne Australia
Disc Herniation
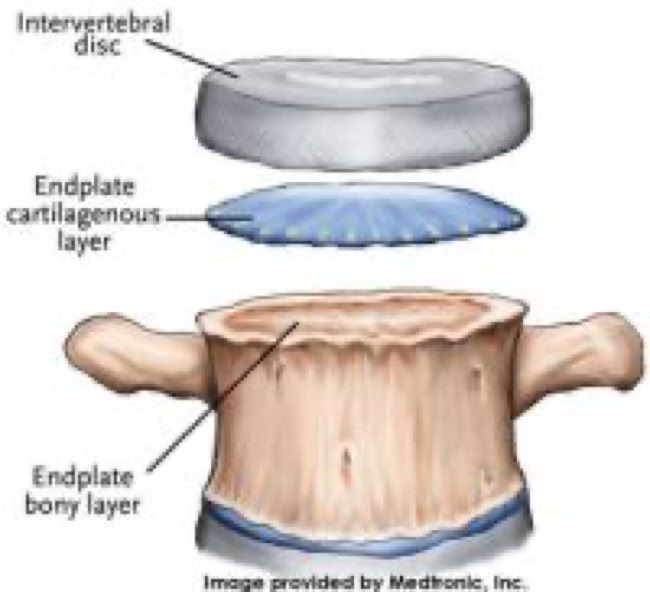
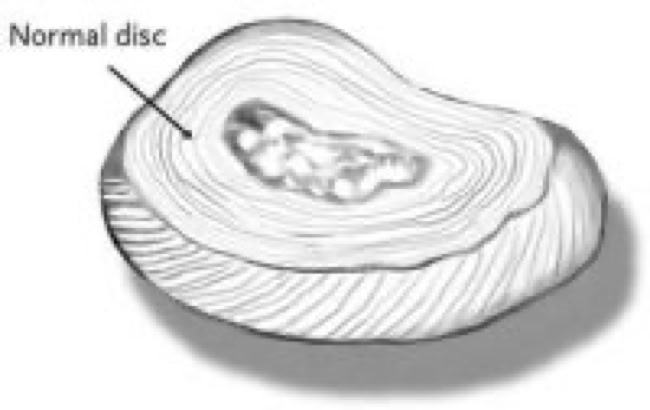
An intervertebral disc is a robust ligament that connects adjacent vertebrae, serving as a crucial shock absorber between each spinal bone. Each disc consists of two primary components: the outer ring of tough fibers, known as the annulus fibrosus, and the soft, gel-like center, called the nucleus pulposus. The annulus is the disc's most resilient part, acting as a ligament that holds the vertebrae together. Meanwhile, the nucleus is hydrated and primarily functions as the spine's shock absorber, helping to cushion the forces exerted on the spine.
As the spine extends from the neck to the lower back, the discs increase in size to accommodate the growing demands of shock absorption due to the effects of gravity and body weight. The role of these disc ligaments mirrors that of the ligaments in the knee or shoulder: they allow for movement and flexibility, enabling the spine to bend forward, backward, and sideways. Like all ligaments, intervertebral discs can be vulnerable to injury.
DISC INJURY
The annulus of the disc can tear or rupture at any point around its perimeter. If the tear occurs without any disc material escaping, it’s known as an annular tear. This can be extremely painful since the outer fibers of the annulus transmit pain signals. Though the tear will gradually heal with scar tissue, it remains more susceptible to future injury or additional tears.
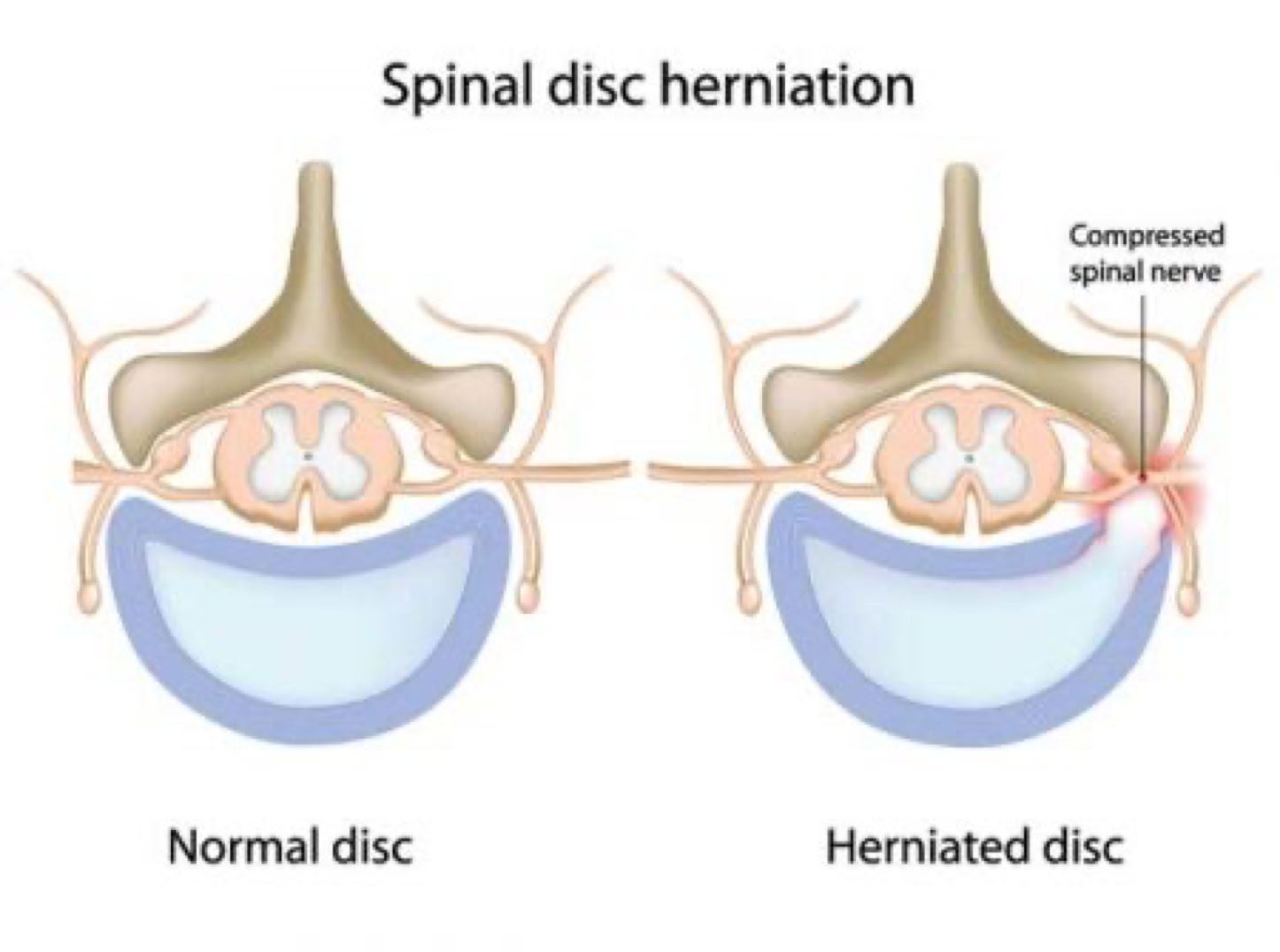
If the annulus tears and the inner nucleus of the disc is pushed out, a portion of the disc can break off and extend beyond its usual boundaries. This results in a disc herniation, which is defined as the displacement of disc material beyond the normal limits of the disc space. Terms like "disc protrusion," "disc bulge," "disc herniation," "ruptured disc," and "slipped disc" all refer to the same condition—when disc material extends outside its normal space.
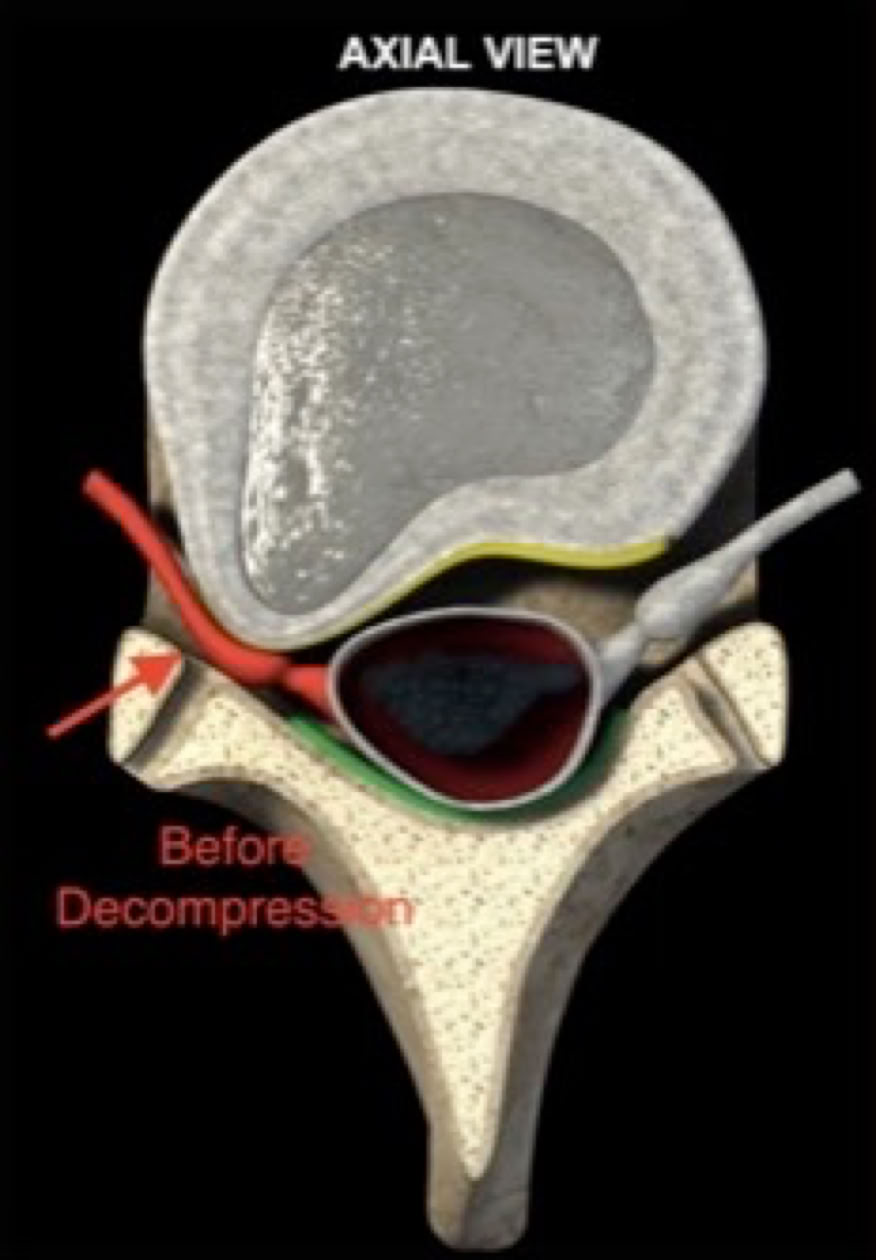
When disc material herniates, it can compress the spinal cord or nearby nerve roots, leading to intense pain along the affected nerve’s path. Pressure on a nerve root from a herniated disc may cause numbness, weakness, and a deep, aching pain, or even sharp, shooting pain that radiates down the nerve pathway. Additionally, the nucleus pulposus (the center of the disc) is known to be acidic, which can chemically irritate the nerve roots.
Discs themselves have two distinct parts: the tough, outer annular portion and the soft, central nuclear portion. A disc herniation is often compared to the consistency of lobster or crab meat, given its soft yet potentially irritating nature.
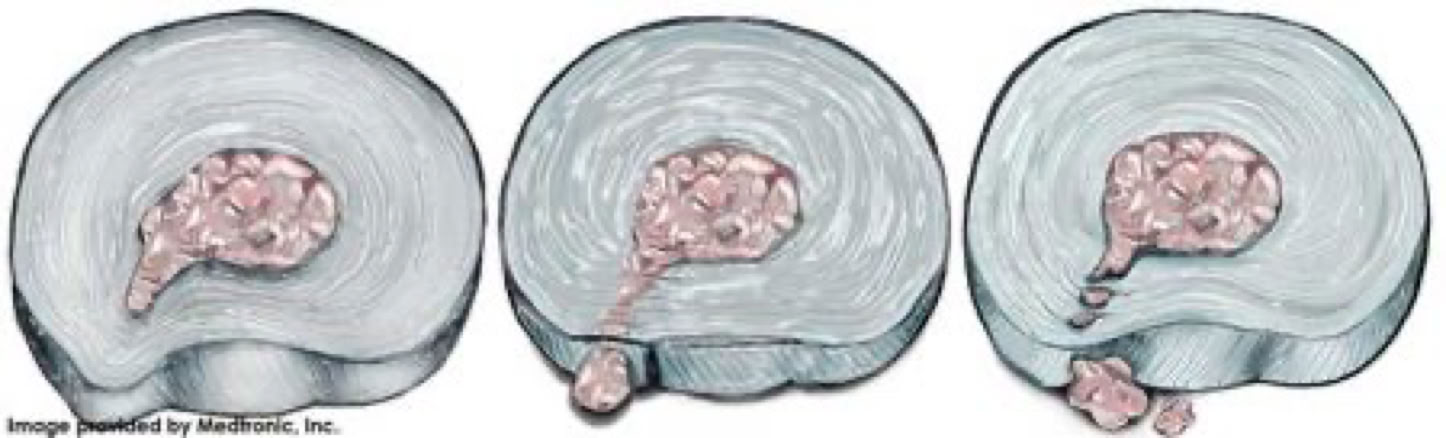
VARYING LEVELS OF A DISC HERNIATION
A disc fragment in the neck that compresses a nerve can lead to pain radiating down the arm. Similarly, if a piece of disc material breaks off in the lower back and presses on a nerve serving the lower extremity, it can cause leg pain. This can also occur in the mid-back, resulting in pain that wraps around the trunk. The specific pain pattern depends on which nerve is affected. For example, classic sciatica—pain running down the back of the thigh and calf—is often the result of a herniated disc in the lower spine, particularly at the L5 and/or S1 levels, which pinch the corresponding nerve and produce this distinctive pain pattern.

Causes
Herniated discs are most common in young to middle-aged adults, though they are rare in children. A herniated disc typically occurs when excessive force is applied to an otherwise healthy intervertebral disc. Even a healthy disc may struggle to absorb significant pressure, particularly in the neck or lower back. For instance, falling from a height, such as from a ladder, can generate enough force to damage the spine. This may lead to a vertebra breaking or a disc rupturing. Similarly, bending and lifting heavy objects places high pressure on the discs between the vertebrae, potentially causing a rupture if the force is too great.
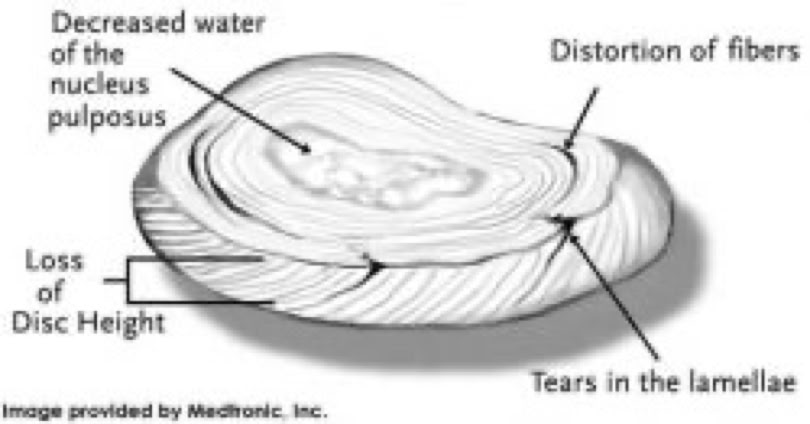
Additionally, repeated stress on the disc can cause gradual damage. Over time, tears in the outer layer of the disc weaken it, making it more susceptible to rupture under pressure. Activities that would have posed no problem years earlier can, over time, become too much for the disc to handle. This is often due to the natural aging process, which leads to degenerative changes in the spine. As we age, the discs lose water content, become less flexible, and lose their ability to absorb shocks. Not everyone with a herniated disc has degenerative disc disease, and not everyone with degeneration will develop a herniated disc.
Poor posture can also contribute to disc herniation. When postural muscles become fatigued, the shoulders round forward, and the head drifts forward. This places excessive strain on the discs, ligaments, and joints of the cervical spine. Even a slight forward head posture adds significant pressure on the spine. For instance, for every inch the head shifts forward, there’s an additional 10 pounds of pressure on the cervical spine. Over time, this can lead to disc weakness, inflammation in the joints and ligaments, and muscle tightness.
Symptoms
The symptoms of a herniated disc vary but are often due to increased pressure and irritation of the nerves. In many cases, people may not experience neck or back pain. Instead, symptoms commonly include pain radiating into one or both arms or legs, numbness or tingling in the extremities, muscle weakness, and a loss of reflexes. The location of these symptoms depends on where the herniation occurs, as nerves follow specific patterns in the body.
Diagnosis
A herniated disc is typically diagnosed following a comprehensive medical history and physical examination. Imaging tests are often the next step in understanding the underlying spine pathology.

LUMBAR DISC HERNIATIONS ON MRI
Treatment Options
At our clinic, the treatment of a herniated disc primarily involves Non-Surgical Spinal Decompression. This therapy focuses on gently creating space between the vertebrae, a process known as distraction. By doing so, it generates negative pressure within the affected disc, helping to pull the herniated material away from the compressed nerve. This approach offers an effective, non-invasive alternative to surgery, aiming to reduce pain and promote healing.
© 2025 Dr. Ilan Sommer DC (USA), Phone# 1300662295 Send us an Email